The gut microbiota is proving to play a central role in human health. The term “human microbiota” refers to the billions of microorganisms that live inside and on our bodies. Examples include those present on the skin, in the eyes, respiratory tract, urogenital tract, and most importantly, the gastrointestinal tract. The term “microbiome” refers to the collection of genes of the microbiota.
What is the gut microbiota?
It is the collection of microorganisms that populate the digestive tract. It consists of billions of bacteria, viruses, fungi, and protozoa that communicate with each other and perform important functions for our health. The Bacteriota is the part composed of bacteria, Virota is the part composed of viruses, and the Mycota is the part represented by fungi. However, when we talk about the gut microbiota, we generally refer to the bacterial part due to the bacteria’s greater ability to metabolize the products of digestion. Bacteria act an important role in the final metabolization (fermentation) of carbohydrates and proteins. From these processes derive different metabolites, such as short-chain fatty acids (SCFAs), hydrogen, carbon dioxide, ammonia, amines, phenols, and energy.
What are its main functions?
The exchange of mutual benefits is the base of the coexistence between us and the microorganisms that inhabit our intestines. We provide the nutrients, and the gut microbiota performs various functions that contribute to our physical and mental well-being.
The main functions of the gut microbiota are:
- Physiological activities: It ensures the proper functioning of the digestive tract.
- Metabolic activities: It regulates the sensation of satiety and modulates the concentration of glucose and cholesterol in the blood, the synthesis of amino acids, the metabolism/recycling of bile acids, the metabolism of polyphenols and antioxidants, energy production, and vitamin production.
- Modulation of the immune system: It regulates the development, homeostasis, and function of innate and adaptive immune cells.
- Defense against pathogens: It inhibits their growth by consuming available nutrients and/or producing bacteriocins (antibacterial metabolites).
- Elimination of toxins and waste products from the intestinal lumen.
- Maintenance of intestinal barrier integrity: It also prevents the invasion of pathogenic bacteria.
- Neuroendocrine modulation: The main neuroendocrine system of the body, which controls various bodily processes in response to stress, the hypothalamic-pituitary-adrenal axis, interacts with the gut microbiota. Furthermore, the vagus nerve, which acts as a link between the central nervous system and the enteric nervous system, expresses receptors for intestinal peptides that the gut microbiota can regulate.
- Regulation of the gut-brain axis: The gut microbiota can exert a strong influence on the functions of our brain, but it is also influenced by it. It creates a continuous connection known as the microbiota-gut-brain axis.
A healthy gut microbiota is therefore the best ally for our health.
What is a “healthy” gut microbiota?
The distinction between “good bacteria” and “bad bacteria” is not so clear-cut. In fact, some strains can be harmful or not depending on their location/abundance. Strains that are always pathogenic do not belong to our microbiota but can infect our intestines. This can happen through ingestion with contaminated food or water.
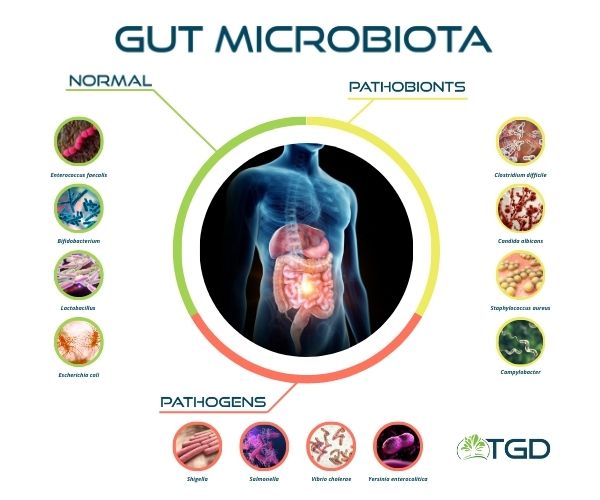
A healthy gut microbiota consists of diverse species, with a predominance of beneficial ones, in balance with each other and with the intestine that hosts them. “Eubiosis” is the name for this state of balance. This balance can alterate under certain conditions. This leads to an alteration of the microbiota, known as “dysbiosis.”
Dysbiosis has been associated with many conditions, including obesity, chronic inflammatory bowel diseases, and other dysfunctions such as immune and metabolic disorders.
We can measure the health of our gut microbiota using three criteria:
- Species richness
- Relative abundance of each species
- Ratio between beneficial and potentially harmful species

What does the “health” of our microbiota depend on?
The health of our gut microbiota depends on various factors, such as the environment we live in, our diet, and our lifestyle. The type of birth and breastfeeding also influence our gut microbiota. Natural birth and breastfeeding represent important moments for the development of a healthy and rich gut microbiota in newborns, with implications that can last a lifetime.
Our diet can greatly influence the gut microbiota. A diet rich in fruits, vegetables, and fiber, such as the Mediterranean diet, is associated with a diverse and healthy microbiota, which has anti-inflammatory effects. On the contrary, diets rich in processed and industrial foods, simple sugars, and saturated fats are associated with the development of a pro-inflammatory gut microbiota responsible for the development of chronic diseases.
How variable is it?
The human gut microbiota consists of a complex community of over a trillion bacteria belonging to 500-1,000 different species. Its composition varies from one population to another, from one individual to another within the same population, and even within the same individual at different stages of life and throughout the day! In fact, the gut microbiota can transiently change about 60% of its composition within a single day. The remaining 40% tends to remain stable in the central part of life but is unstable during infancy (when the maturation process is ongoing) and in old age. For this reason, these age groups are considered “fragile” and more exposed to risks.
The stable part of the gut microbiota has the priority on the utilization of available nutrients and occupies exclusive spaces (niches). The variable part is more sensitive to environmental and dietary variations. So it competes with the stable part for colonization of the digestive tract. This competition does not favor the most recently introduced microorganisms, which fail to stably colonize the digestive tract. This is why the supplementation of probiotics often does not achieve the desired effects.
How is the bacterial component composed?
Bacteria are classified into broad groups called Phyla (Phylum in singular), which are further divided into smaller groups where bacteria with increasingly similar characteristics are grouped.
The classification scheme is as follows: Phylum, Class, Order, Family, Genus, Species.
The majority of bacteria in our gut microbiota belong to six phyla: Firmicutes, Bacteroidetes, Actinobacteria, Proteobacteria, Fusobacteria, and Verrucomicrobia.
Firmicutes and Bacteroidetes represent 90% of the gut microbiota. The Firmicutes phylum includes over 200 different genera, such as Lactobacillus, Bacillus, Clostridium, Enterococcus, and Ruminicoccus. Intestinal Bacteroidetes, on the other hand, mainly belong to two genera: Bacteroides and Prevotella.
Actinobacteria are less abundant and primarily represented by the genus Bifidobacterium.
The most common species belong to three genera: Bacteroides, Prevotella, and Ruminococcus. The prevalence of one of them defines three “types” of gut microbiota called enterotypes.
- Enterotype 1: Bacteroides prevalence
- Enterotype 2: Prevotella prevalence
- Enterotype 3: Ruminococcus prevalence
An enterotype is a functional association of different bacterial species. Each enterotype is not a well-defined identity, but it remains stable in adulthood and can be restored if altered. The enterotype of the gut microbiota influences our metabolism. For example, Bacteroides produce more vitamin C, B2 (riboflavin), B5 (pantothenic acid), and H (biotin). Prevotella produces more vitamin B1 (thiamine) and folic acid.
Enterotypes are greatly influenced by environmental factors, especially our diet!
Author: Dr. Ilaria Maria Saracino
